21st Century Advanced Technology
Tomorrow’s Dentistry Today!
Our mission statement at Tuckerton Dental is to provide an outstanding experience for all the dental implantology needs of our loyal and trusting patients by offering:




Mastership & Fellowship – Resnik Implant Institute
Board Certified Diplomate & Fellow – International Congress of Oral Implantologists
Master & Fellow – Academy of General Dentistry
Diplomate & Fellow – International Academy of Mini Dental Implants
Master & Fellow – American Academy of Implant Prosthodontics




Fellow – Misch International Implant Institute
Associate Fellow & Diplomate – American Academy of Implant Dentistry
Diplomate – Global Mini Dental Implant Association
Fellow – Institute for Advanced Laser Dentistry
Fellow – American Academy of Small Diameter Implants
Fellow – International Congress of Oral Implantologists
Fellow – Academy of General Dentistry
Specialty in Prosthodontics, Specialty #3495
Registered Dental Hygienist
April 26, 2024 – Tuckerton Dental, Tuckerton, NJ
Join Dr. Petrosky for this Hands-on One Piece Series workshop where he will detail how this simplified, practical, and versatile approach to implants can improve your practice and workflow. This workshop will go over: single, multiple, and full-arch applications, immediate placement examples, minimally invasive oral surgical techniques, and the advantages of One Piece implants. It also provides 7 continuing education credits.


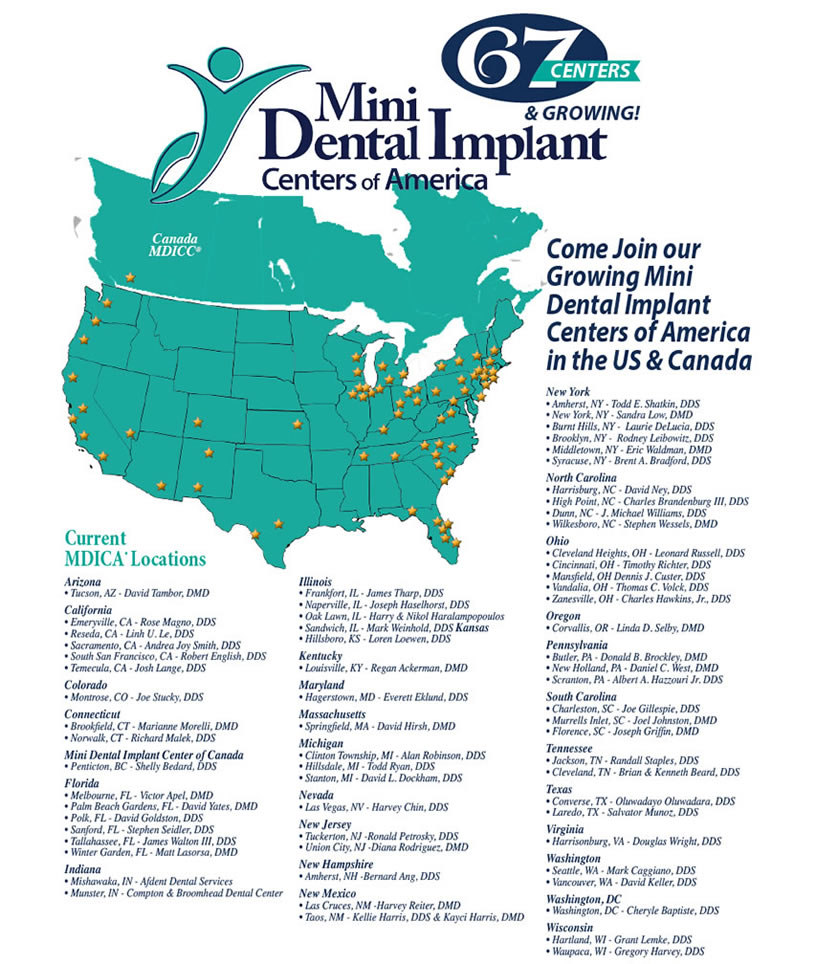
Tuckerton Dental provides the revolutionary benefits of mini dental implants!
Having trouble with your dentures? Are you missing one or more teeth? Then, mini dental implants may be for you!


Cosmetic dentistry isn’t just for movie stars! New techniques allow us to reshape your smile with minimal changes to your natural teeth. See our cosmetic dentistry page to see how subtle changes can make a dramatic impact on the way you look and feel.
LANAP – LASER PERIODONTAL THERAPY™ of New Jersey, is an amazing breakthrough in periodontal treatments, the alternative to gum “flap surgery” License No. 08037. The way to repair gum damage is to get rid of the infection and close up the pockets. Until now, that meant surgery and sutures. But today, many dentists offer LASER PERIODONTAL THERAPY™, a patient-friendly, minimally-invasive procedure that’s a great improvement over standard gum surgery.
Technology today is changing everyday lives. Many people, however, aren’t aware that technology also in impacting dentistry in new and exciting ways. Cutting-edge innovations in dental instruments are requiring less time in the dental chair, causing less discomfort and creating satisfying results. One breakthrough instrument, called CEREC, allows dentist to quickly restore damaged teeth with natural-colored ceramic fillings, saving patients time and inconvenience.
Laser Dentistry of New Jersey featuring POWERLASE® AT Spa… the World’s Most Versatile Dental Laser for Superior Performance
Laser Research introduces the Lares PowerLase AT dual -wavelength laser, which combines dentistry’s best two wave lengths in a single system for superior hard and soft-tissue cutting performance. The PowerLase AT features the Freedom-Balanced articulated arm, which transmits laser energy 10 to 15 times more efficiently. This feature, combined with the 20-watt power supply and VPC technology, allows the PowerLase AT to cut tooth faster than a high-speed handpiece. This laser has received FDA 510(k) clearance to market for a wide variety of indications.


The i-CAT, the leader in Cone Beam 3-D Dental Imaging for dental applications only provides high-definition, digital imaging at reduced cost with less radiation to the patient and a typical scan time of only 8.5 seconds. The i-CAT’s computer controlled software delivers quick & easy reconstruction of critical anatomical information typically in under 30 seconds.